Specific Genes Predict HCV Treatment Success
Identification of specific genes predicts which patients will respond to Hepatitis C treatment
Toronto, Ontario, May 2 /PR Direct/ –
Simple blood test in the near future possible
(Toronto, May 2, 2005) – For the first time, physicians at University Health Network and University of Toronto have identified a small subset of genes that can predict whether a patient with chronic Hepatitis C will be able to respond to current treatments.
These genes could also become the basis of a simple new test in the future to predict which patients will respond to therapy.
The study, published in the May issue of the American Gastroenterological Association’s Gastroenterology, found that the difference between those patients who responded to treatment and those who did not was the level of expression – whether the genes were turned on or turned off – of 18 genes.
“Our results demonstrate that a relatively small number of genes can predict response to therapy. These genes may be important to the ability of the patient to eliminate the virus, so studying these genes in more detail will hopefully lead to novel antiviral treatments,” said Dr. Ian McGilvray, the senior author of the study. Dr. McGilvray is a transplant surgeon at Toronto General Hospital, University Health Network and an Assistant Professor of Surgery at the University of Toronto. “By manipulating the products of these genes we might be able to improve treatment responses to this chronic disease.”
“This information is helpful for patients because it’s one more piece of evidence that we hope will encourage ‘responder’ patients to start and continue treatment for Hepatitis C, despite it’s many side effects,” said Dr. Jenny Heathcote, a hepatologist at Toronto Western Hospital, University Health Network and Professor of Medicine at University of Toronto, who contributed to the study and treats many of the patients in the study. “We want to be able to give patients as much information as we can, so that they can make the best decisions about their treatment options.”
Tony Angelini, 42, was one of the patients in the study who responded to treatment. He is now clear of the virus. “Knowing that you are a responder gives you the courage and the fight to go on. It was devastating, but having the support of my friends and hospital staff really helped me through the treatment. And I wanted to participate in this study so that the research could help others in the future.”
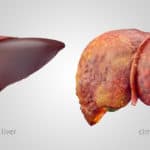
The study followed 31 patients with chronic Hepatitis C who were treated at Toronto Western Hospital from October 2001 until May 2004. Hepatitis C is a disease of the liver caused by the hepatitis C virus (HCV). About 230,000 Canadians are infected with it, and about 170 million people worldwide. Over time the viral infection leads to liver damage, cirrhosis and/or liver cancer. It is currently the leading indication for liver transplants.
Liver biopsies were performed on the 31 chronic HCV patients before treatment, and were compared to 20 biopsies from healthy, uninfected livers. 16 patients did not respond to subsequent treatment, while 15 did; both groups were well matched with respect to age, HCV viral load (number of viral particles circulating in the blood), and liver disease activity.
In order to define which genes discriminate between those patients who respond to therapy to those who do not, microarray technology, based in a Banting and Best Department of Medical Research laboratory at University of Toronto, was used to analyze the pattern of genes in all participants. This technology allows scientists to compare levels of expression for tens of thousands of genes on a glass slide – these “gene chips” are the size of a postage stamp. The technology is able to quickly scan the expression of those genes and differentiate between genes which are “turned on” or “turned off”. Comparing “genetic fingerprints” allows researchers to rapidly and effectively identify sensitive genetic changes associated with various stages of disease, and hopefully identify the most suitable candidates for specific therapies.
“We went into this experiment without any hypothesis about what to look for,” said Aled Edwards, a Professor in the Banting and Best Department of Medical Research at University of Toronto with cross appointments in the Departments of Medical Biophysics and Medical Genetics and Microbiology. He is also a senior scientist at the Clinical Genomics Centre at the University Health Network and Director and CEO of the Structural Genomics Consortium. “We cast a very wide net, looking at 19,000 genes of each of the patients.”
The researchers found that the difference between those patients who did not respond to therapy to those who did was a subset of 18 genes. In the non-responders to treatment, 16 genes were turned on and two were turned off. Many of the 16 genes which were turned on are stimulated by interferon, one of the key antiviral agents that the body produces in response to viral infection and a medication that patients currently receive as part of their therapy. “Paradoxically, in the non-responders, the liver is revved up and the genes are responding like mad, but there is something about the response that just does not work,” said Dr. McGilvray.
In the near future, determining the levels of a small subset of genes in patients’ liver biopsies, with perhaps a simple blood test, may be helpful in deciding who will respond to treatment of chronic Hepatitis C with the current combination therapy using the synthetic antiviral agent ribavirin and interferon. This treatment can currently get rid of the virus in only roughly 50% of persons infected with genotype 1, the most common genotype in North America and world-wide.
The study was supported by grants from the PSI Foundation and the Canadian Institute of Health Research.
University Health Network consists of Toronto General, Toronto Western and Princess Margaret Hospitals. The scope of research and complexity of cases at University Health Network has made it a national and international source for discovery, education and patient care. It has one of the largest hospital-based research programs in Canada, with major research projects in transplantation, cardiology, neurosciences, oncology, surgical innovation, infectious diseases, and genomic medicine. University Health Network is a teaching hospital affiliated with the University of Toronto.